Below is a more comprehensive breakdown across key areas of fistula, also known as Anastomosis understanding—from definition to recovery. Each point has been expanded with clarity, supported by expert insight from Dr. Satveer Singh, Consultant Surgical Oncologist (Breast) & Laparoscopic & Endoscopic Surgeon at Sri Harikrishan Nursing Home. ( Best general surgeon in Hazaribagh )
1. What Is a Fistula?
A fistula is an abnormal connection between two body parts, such as organs, vessels, or the skin. While some may occur internally—like between the intestine and skin—others can connect organs in troubling ways (e.g., bowel to bladder). Anastomosis often emerge due to persistent inflammation, infection, surgery, trauma, or chronic diseases like Crohn’s. Accurate diagnosis and timely treatment are essential to avoid complications such as infection or incontinence. Patients often have questions, and under the expert care of Dr. Satveer Singh, they receive thorough evaluation and tailored management.
2. Common Types of Fistulas
- Anal (Anorectal) Fistulas: These form when an infection or abscess in the anal glands creates a drainage path from the anal canal to the skin.
They are classified based on their route relative to sphincter muscles:- Submucosal
- Intersphincteric
- Transsphincteric
- Suprasphincteric
- Extrasphincteric.
- Enterocutaneous Fistulas: Abnormal passages between the intestine and skin, often complications of surgery or infection.
- Enteroenteric/Enterocolic Fistulas: Internal connections between segments of intestines or between the intestines and colon.
- Vesicovaginal / Rectovaginal Fistulas: Occur between bladder and vagina or rectum and vagina, often after childbirth injuries or surgery.
- Bronchopleural Fistula: A lung-to-pleura connection, typically post-surgery or due to infections like tuberculosis.
- Dural Arteriovenous Fistulas: Abnormal vascular connections between arteries and veins in the brain’s dura mater, sometimes manifesting neurological symptoms.
3. Causes & Risk Factors
Anastomosis arise due to:
- Persistent infections or abscesses (common in anal Anastomosis)
- Chronic inflammatory conditions like Crohn’s disease
- Obstetric trauma or prolonged labour leading to vaginal Anastomosis
- Surgical or radiation injuries, or infections in any body region
- Congenital or vascular malformations (notably in cerebral dural Anastomosis)
- Ongoing infections or abscesses (common in anal and enterocutaneous types)
- Inflammatory diseases such as Crohn’s
- Surgery or trauma to pelvic organs
- Childbirth injuries
- Radiation exposure
- Congenital or infectious conditions like tuberculosis
4. Symptoms to Watch For
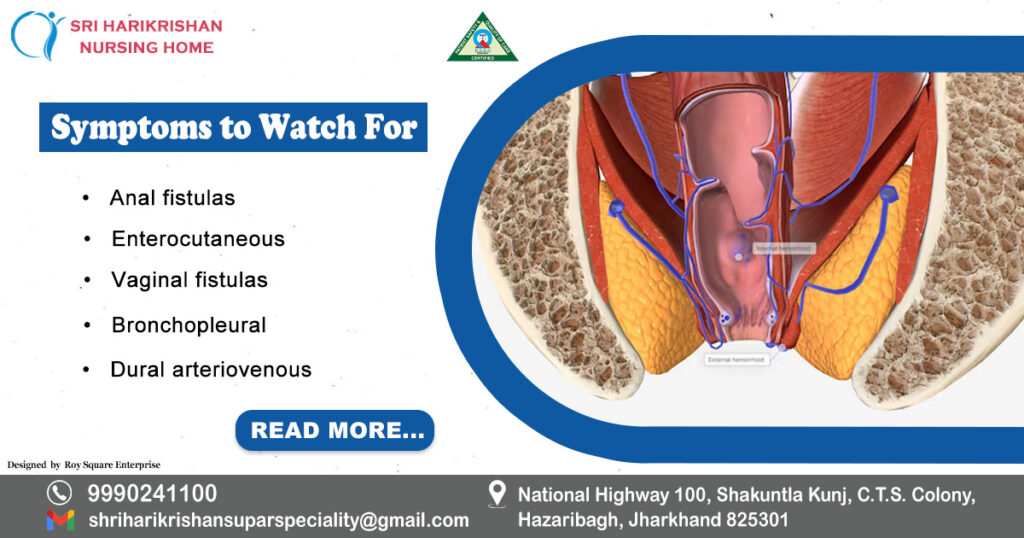
Symptoms vary by Anastomosis type:
- Anal fistulas: Chronic drainage, pain near the anus, swelling, irritation, or fever.
- Enterocutaneous: Gut contents leaking through the skin, foul odor, potential skin breakdown.
- Vaginal fistulas: Leakage of urine or stool through vagina, odor, infection, and discomfort.
- Bronchopleural: Persistent coughing, air leaks, and respiratory distress.
- Dural arteriovenous: Headaches, vision changes, cognitive symptoms, or tinnitus.
5. How Are Fistulas Diagnosed?
Diagnosis often includes:
- Patient history and physical exam, noting drainage or openings.
- Imaging tools:
- MRI or endoanal ultrasound (for anal Anastomosis).
- Fistulography using contrast agent to map tract paths.
- Colonoscopy or sigmoidoscopy if inflammatory bowel disease is suspected.
- CT or MRI for internal Anastomosis like vesicovaginal or bronchopleural types.
- Angiography for Dural AV Anastomosis.
6. Treatment & Management

Treatment depends on type and severity:
- Anal fistulas: Most require surgery due to chronic drainage. Options include fistulotomy, LIFT, advancement flaps, seton placement, or fibrin glue/plugs.
- Enterocutaneous and vaginal Anastomosis: Often need surgical repair, sometimes using grafts or flaps; nonsurgical closure possible in uncomplicated cases.
- Bronchopleural fistula: May require surgery or endoscopic repair, depending on size and symptoms.
- Dural AV Anastomosis: Managed via endovascular embolization, surgery, or radiosurgery.
Anal Fistula Treatment options:
- Fistulotomy (opening the tract)—effective for simple types
- LIFT procedure, seton placement, advancement flaps—for complex cases
- Fibrin glue or collagen plugs—minimally invasive options
Enterocutaneous Fistula
Management includes:
- Stabilizing fluids, infection control, nutrition (often TPN)
- Conservative care may lead to spontaneous closure in ~37%
- Surgery after stabilization, with closure rates >90% in experienced centers
Rectovaginal Fistula
- Wait for inflammation to subside (3–6 months)
- Use setons, antibiotics, or biologics like infliximab for Crohn’s
- Surgical repair with flaps or grafts; colostomy in complex cases
7. Recovery & Outlook
- Post-treatment recovery varies by type; anal Anastomosis surgery may involve wound care and follow-up for incontinence monitoring.
- Seton techniques help gradual healing while preserving muscle continence.
- Other Anastomosis require individualized strategies for healing and prevention of recurrence. Specialist follow-up—including from Dr. Satveer Singh—ensures comprehensive care.
8. Myth vs. Fact: Top 10
| Myth | Fact |
| 1. Fistulas always go away without treatment. | Most require surgical intervention to heal. |
| 2. Only surgery can cause a Anastomosis. | Many arise from infections or chronic diseases like Crohn’s. |
| 3. All fistulas are anal. | They can form in various body parts. |
| 4. Antibiotics cure Anastomosis. | Treat only infection, not structural opening. |
| 5. Fistulas don’t cause serious problems. | They can lead to incontinence, abscesses, or malnutrition. |
| 6. Surgery always causes incontinence. | Techniques like LIFT and setons preserve continence. |
| 7. Only adults get Anastomosis. | Can occur at any age, especially post-surgery or birth trauma. |
| 8. Non-invasive means no surgery. | Some require conservative approaches; others must be fixed surgically. |
| 9. Setons are painful permanent devices. | Temporary, help healing, and are well-tolerated. |
| 10. Once treated, they never recur. | Recurrence is possible; follow-up is crucial. |
9. Top 10 FAQs
- Can Anastomosis heal on their own?
Rarely—some simple submucosal types may, but most require intervention. - Are they always caused by infections?
Not always; trauma, surgery, or chronic disease can cause Anastomosis too. - Is surgery the only option?
For many types, yes—but nonsurgical options exist for mild cases. - Can fistulas return after surgery?
Yes; monitoring and follow-up reduce recurrence risk. - How long is recovery?
Varies—anal fistula recovery may take weeks; internal Anastomosis depend on location and complexity. - Will I lose function in the affected area?
Modern techniques aim to preserve muscle and organ function. - Do fistulas always cause pain?
Not always; some cause minimal symptoms like leakage or irritation. - What complications can arise if untreated?
Chronic infection, abscesses, incontinence, or nutritional issues. - Can fistulas affect fertility or childbirth?
Some types like rectovaginal Anastomosis may require special obstetric care. - Who should manage fistulas?
A specialized surgeon—like Dr. Satveer Singh at Sri Harikrishan Nursing Home—, ensures expert diagnosis, treatment, and follow-up care.
Final Thoughts
Anastomosis are complex medical conditions that demand a targeted, expert-led treatment approach. Whether anal, enterocutaneous, vaginal, or arteriovenous in nature, accurate diagnosis and individualized management are vital. With advanced surgical methods and compassionate care, particularly under trusted professionals like Dr. Satveer Singh, relief and recovery are well within reach.
